Now is a really good time to focus on carbapenem-resistant bacteria. We have spent much of the past 3 years focusing on one particular virus. But now that the clinical issues linked to SARS-CoV-2 are waning for our hospital patients, the threat of carbapenem-resistance in Gram-negative bacteria comes to the fore. An excellent study with far-reaching consequences has been published from Italy. Carbapenem resistance is bad news if you have a BSI: patients with carbapenem-resistant BSI were roughly twice as likely to die as patients with carbepenem-susceptible BSI.
Continue readingcarbapenemase
Can you GES which carbapenemase caused this CPE outbreak?
An unusual and interesting outbreak of CPE was published recently in Clinical Infectious Diseases. Several key points: don’t rely solely on a PCR detecting the “Big 5” carbapenemases (NDM, KPC, OXA-48, IMP, VIM) – at some point you need to test for phenotypic carbapenemase activity; WGS can really help us in unravelling complex transmission routes; and covert plasmid propagation within and between species is a reality.
CPE contamination of hospital wastewater: smoking gun or innocent bystander?
A recent US study has investigated CPE contamination of sinks, drains, and wastewater. Carbapenemase-producing bacteria were identified throughout the drainage and water system, from drains in patient rooms, right through to wastewater sampled through manholes adjacent to the hospital. My main question in all of this is whether this huge reservoir of carbapenemases in hospital wastewater is a risk for patients. The lack of genetic similarity between isolates in hospital wastewater and isolates from patients suggest not, but I suspect there’s an indirect link and these carbapenemases find their way into isolates affecting humans, which is supported by genetic links between the plasmids carrying the carbapenemases.
Looking back on a CPE plasmid attack in the Northwest of England
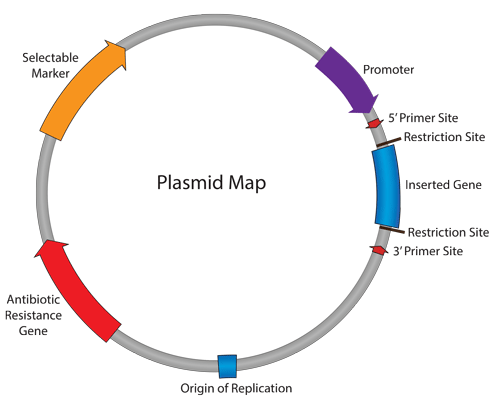
A genomic study of 44 isolates of CPE from various species identified between 2008 and 2010, mainly from the Northwest of England, has concluded that plasmids played a key role in the early dissemination of CPE.
Promiscuous plasmids: a rapid reflection from ECCMID 2017
I came to ECCMID 2017 with a very specific question: do we need to think beyond ‘same-bug-same-gene’ horizontal transmission from a practical IPC view point in order to address the threat of IPC? The answer, unfortuantely, is yes!
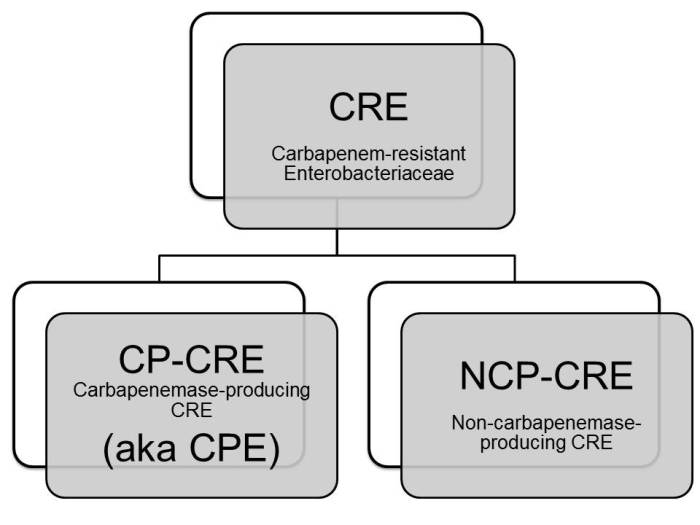
Acronyms for carbapenem-resistant bacteria (again)
I am currently involved in some research that requires a clear distinction between CPE (i.e. Enterobacteriaceae that produce a carbapenemase) and non-carbapenemase-producing CRE. Since ‘non-carbapenemease-producing carbapenem-resistant Enterobacteriaceae’ is a bit of a mouthful, I need to come up with some sort of acronym. I would appreciate your thoughts on the scheme set out below:
You can read more thoughts on acronyms for carbapenem-resistant bacteria in a previous post here.
The carbapenemase is out there
A PNAS paper on the genomic diversity of carbapenemase producing bacteria in the US reports strong evidence of carbapenamase (an enzyme produced by bacteria that breaks down carabapenem antibiotics) activity but no sign of a carbapenemase gene. This provides a timely reminder that we are only really scratching the surface in our understanding of carbapenemases and how they work.
KPC Casanova carbapenemase
The risk of interspecies transmission of carbapenemase genes is a real concern. We can barely get our heads around many different types of carbapenemase in a whole host of Gram-negative bacteria (compare the relative simplicity of methicillin resistance in S. aureus: a single gene, in a single species). Throw in interspecies horizontal transmission of carbapenemases and things get really tricky! Do we implement different control strategies to try to interrupt the transmission of carbapenemases (in contrast to the organisms themselves)? Could you have a multispecies outbreak of a carbapenemase on your hands and not even realise it?
Antibiotic Awareness: background and links
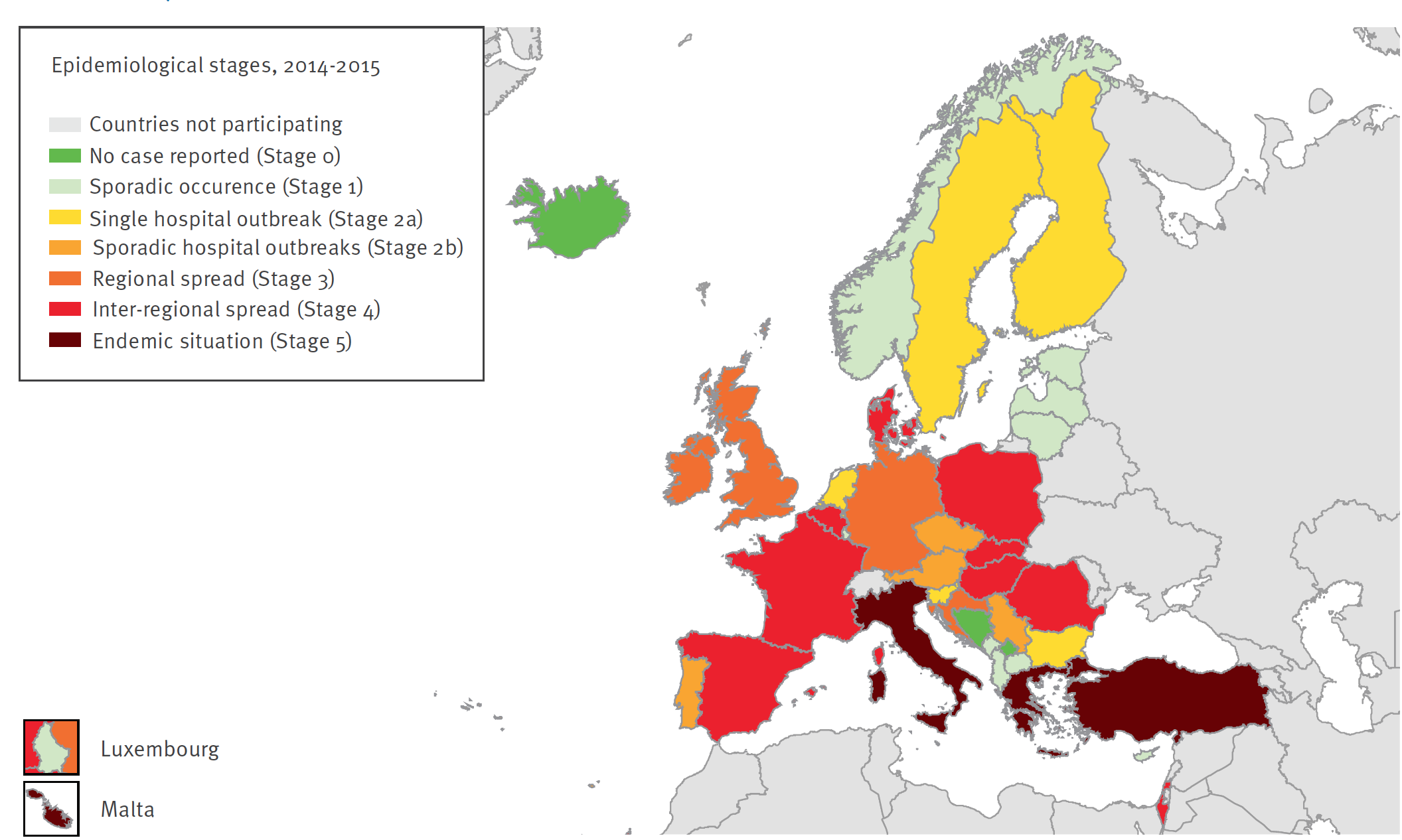
European Survey of Carbapenemase-Producing Enterobacteriaceae (EuSCAPE) project
The EuSCAPE project aimed to improve understanding of the occurrence and spread of CPE. LINK
About European Antibiotic Awareness Day
European Antibiotic Awareness Day is a European health initiative coordinated by ECDC which aims to provide a platform and support for national campaigns on the prudent use of antibiotics. Each year across Europe, the European Antibiotic Awareness Day is marked by national campaigns on the prudent use of antibiotics during the week of 18 November. Prudent use means only using antibiotics when they are needed, with the correct dose, dosage intervals and duration of the course. Follow the European Antibiotic Awareness Day: #EAAD. http://antibiotic.ecdc.europa.eu
About World Antibiotic Awareness Week
The World Health Organization is leading a global campaign for the first World Antibiotic Awareness Week with the slogan “Antibiotics: Handle with Care”. The campaign calls on individuals, governments and health and agriculture professionals to take action to address this urgent health problem. The first World Antibiotic Awareness Week will take place on 16-22 November. Follow the World Antibiotic Awareness Week: #AntibioticResistance. www.who.int/drugresistance.
Continue reading
Appraising the options for detecting carbapenemase-producing organisms
Carbapenemase-producing organisms (including CPE) present important clinical challenges: the “triple threat” of high levels of antibiotic resistance, virulence, and potential for rapid spread (locally, regionally, nationally, and globally)! However, these organisms somewhat ironically also present challenges to detection in the clinical laboratory. You’d expect that since these organisms are so important clinically they’d be dead easy to detect in the clinical lab – but this isn’t the case.
A comprehensive review published in Clinical Microbiology Reviews provides an overview of the diagnostic approaches to detect carbapenemase producers in the clinical lab. Figures 6 and 7 of the review provide a useful overview of the two broad approaches you could take: culturing organisms on agar plates, or using nucleic acid amplification techniques (NAAT – most commonly PCR) directly from a rectal swab.