Curtis Donskey’s group recently published a multicentre randomised trial in 16 US hospitals to evaluate the impact of an enhanced cleaning programme (including fluoruescent markers, environmental cultures, and feedback to cleaners) on the transmission of C. difficile. The intervention resulted in an increase in the removal of fluorescent markers, a reduction in environmental contamination with C. difficile, but no reduction in healthcare-associated CDI!
Author: Jon Otter (@jonotter)
Take care. Not antibiotics.
Mindful of our need to up our game in terms of communication to non-experts around AMR-related issues, I have been scouting around for a good video to portray the basic of AMR, and came across this by Health Education England. It’s not the best animation that I have seen, but I quite like it – and the strap line at the end is interesting (“Take care. Not antibiotics”). I’d be interested in your views on this video, and please feel free to flag any other good ones out there.
Special issue on MDR-GNR
The Journal of Hospital Infection have published a welcome special issue on multidrug-resistant Gram-negative bacteria. The collection includes some updates on epidemiology, staff carriage (again!), clinical microbiology, and patient perspectives on CPE, and is well worth a read.
Staff screening for MDROs: closing Pandora’s Box
A brave study from the Palmore/Frank group at NIH has opened the Pandora’s Box that is screening staff for MDROs, and, I’m delighted to say, firmly closed it with their findings! Only 3% of staff carried ESBLs, one carried a CPE, and none carried VRE, and this despite extensive contact with MDRO patients for many of the staff sampled!
Everybody needs good neighbours (for sharing CPE)
BMC Medicine have recently published a study from researchers in Oxford, PHE, and Manchester illuminating the importance of referral networks in the transmission of CPE. The bottom line is that regional referral networks seem to be the most important driver of CPE spread, such that a small CPE problem close to home is more of a threat than a larger CPE problem in a distant referral network!
Money makes the AMR bugs go round in Europe? A reflection from ECCMID 2017
If you pick an AMR bacterium of your choice, go to EARS-Net and plot prevalence across Europe, in most cases you’ll see a rough ‘north-south’ divide, with northern European countries doing better than southern European countries in terms of AMR rates (e.g. see below for antibiotic-resistant K. pneumoniae). What is driving this difference in AMR rates? A session at this year’s ECCMID asked just that question, hypothesising that weather / climate, economics, patient mix, or culture explain the difference. It was a fascinating session, so I thought I’d share some highlights!
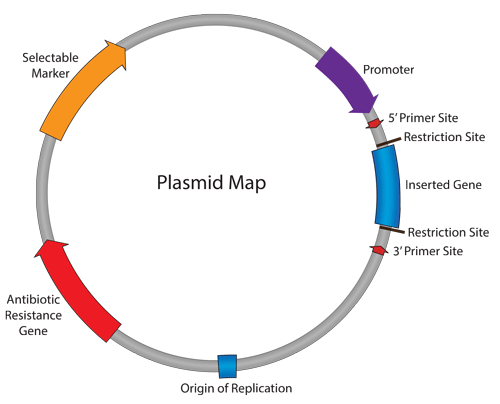
Promiscuous plasmids: a rapid reflection from ECCMID 2017
I came to ECCMID 2017 with a very specific question: do we need to think beyond ‘same-bug-same-gene’ horizontal transmission from a practical IPC view point in order to address the threat of IPC? The answer, unfortuantely, is yes!
CPE: a good reason to avoid surgery in Spain!
A clear simple study has a stark headline: 16% of admissions to a Spanish surgical ICU carry CPE. This sort of carriage prevalence is at a ‘practice-affecting’ level: the empiric antibiotic choices may be altered and you begin to wonder what is left when the first signs of infection develop in almost 1 in every 5 patients…
Going for GNBSI
We’ll be publishing the results of the vote on whether or not we can halve HA-GNBSI by 2021 later this week. Right now, it looks like Martin is heading for a comfortable, if somewhat depressing victory (“No, we can’t halve GNBSI by 2021”) but there’s still time to ride a wave of positivity and vote with me that “Yes, we can halve GNBSI by 2021”. So, I thought that now would be an appropriate time to review the recent JHI paper that both Martin and I referred to, providing some enhanced epidemiological data on E. coli BSIs in England.
Can we really halve Gram-negative BSIs (GNBSIs) by 2021? Kiernan vs. Otter Mk II
The UK government has recently announced their ambition to halve the rate of Gram-negative BSIs by 2021. Looking at the latest mandatory reporting dataset (see Figure 1 below), you can see why. Impressive reductions in MRSA BSI and C. difficile, but a notable increase in E. coli BSI. And this combined this with worrying data around increased antimicrobial resistance in Gram-negative bacteria from the ESPAUR report. In this post, Martin Kiernan and Jon Otter present both sides of the argument as to whether Gram-negative BSIs can be reduced by 2021, with comment from Andreas Voss and Marc Bonten! And you get to vote on which side of the argument you come down on after reading the arguments. Let battle commence…