A fabulous study recently published in JAMA evaluates the ‘Benefits of Universal Glove and Gown’ (BUGG) in US ICUs. This is a model study design: one of the first cluster randomized controlled trials of a non-therapeutic infection control intervention. Twenty ICUs were paired and randomized to either universal glove and gowning, or to continue the current practice of placing patients known to be infected or colonized with MRSA and VRE on contact precautions. The hypothesis is that undetected colonization with MRSA and VRE is common, and the only real way to address this is to assume everybody is colonized!
Summary of findings:
- Universal glove and gowning was not associated with a reduction in a composite measure of MRSA / VRE acquisition (the primary outcome).
- VRE acquisition was not reduced by universal glove and gown use, whereas MRSA was.
- CLABSI, CAUTI and VAP; ICU mortality; and adverse events did differ significantly between the two groups.
- Hand hygiene compliance on room entry was not significantly different between the two arms, whereas hand hygiene compliance on room exit was significantly higher in the intervention arm.
- Healthcare workers visited patients 20% less frequently in the intervention arm (4.2 vs. 5.2 visits per hour).
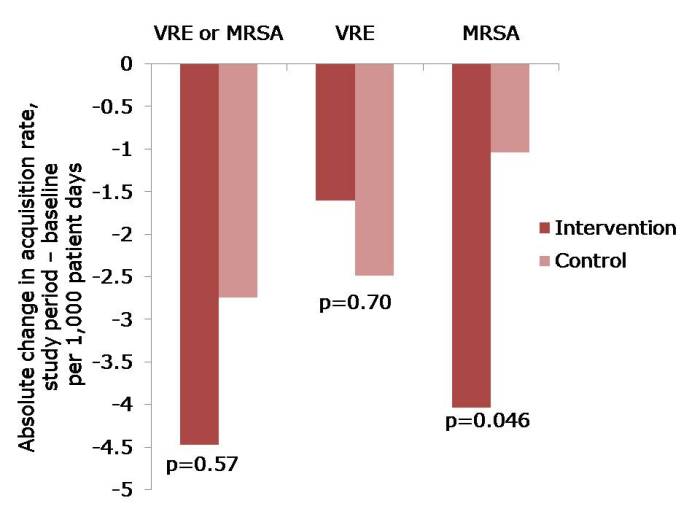 Figure: The change in acquisition rate, comparing the baseline period with the study period for the intervention and control units.
Figure: The change in acquisition rate, comparing the baseline period with the study period for the intervention and control units.
Here’s what’s BUGGing me about this study:
- The acquisition rate in both intervention and control study arms reduced (Figure). The acquisition rate reduction in the control arms may be due to improved compliance with admission screening, resulting in more accurate ascertainment of who required contact precautions.
- The significant reduction was achieved for MRSA but not for VRE. The authors suggest that VRE colonization may have been suppressed on admission and not detected, and flourished during antimicrobial therapy giving the impressive of acquisition. I wonder whether differences in the routes of transmission may also have contributed; for example, VRE seems to be substantially “more environmental” than MRSA. Another potential confounder is that, by chance, the prevalence of MRSA or VRE on admission to the intervention ICUs was more than double that in the control ICUs (22% vs. 9%). In actual fact, the raw rate of MRSA acquisition in the intervention ICUs was marginally higher than in the control ICUs during the intervention period (6.00 vs. 5.94 per 1000 patient days), even though the change in rate was significantly greater on the intervention ICU. Although adjustment was made for this difference in the analysis, it may have skewed the findings somewhat.
- The authors achieved remarkably high compliance with admission screening (around 95%), discharge screening (around 85%) and glove and gowning (around 85%). Each site had the luxury of a study coordinator and a physician champion to lead implementation, plus weekly feedback on screening compliance and visits from study investigators. Most ICUs would not be afforded these luxuries so I suspect that real-world compliance outside of the somewhat artificial study environment would be considerably lower. Indeed, an ID Week poster suggests that compliance with gowning in one US ICU was a ‘dismal’ 20%!
- Adverse events were not significantly higher in the universal glove and gowning arm, which may seem surprising prima facie. However, the reason why adverse events are more common for patients on contact precautions is that they are marginalized by being on contact precautions. If all patients are effectively on contact precautions, the time of healthcare workers would be spread evenly.
- Universal gloving is likely to result in universally bad hand hygiene compliance within the room during patient care; when healthcare workers feel protected, they are less likely to comply with hand hygiene and gloves are a good way to make healthcare workers feel protected. The increase in hand hygiene compliance on room exit is probably also a symptom of inherent human factors, since healthcare workers feel more ‘dirty’ when exiting the room of a patient with a higher perceived risk of MDRO ‘contamination’ (the so-called “urgh” factor).
- Healthcare workers had less time for patient care in the intervention arm because they were busy donning and doffing gloves and gowns. Interestingly, the authors suggest that fewer visits may be a good thing for patients, and may have contributed to their reduced chances of acquiring MRSA. This seems unlikely though, given the fact that VRE acquisition was not reduced. On balance, less contact with healthcare workers is likely to be bad for patients.
- The increased cost of universal glove and gowning was not evaluated and, whilst incrementally small, would be a substantial sum.
In summary, this study sets the standard in terms of rigorous assessment of an infection prevention and control intervention. Universal application of gloves and gowns is unlikely to do as much harm as universal administration of mupirocin, but it will not make a profound reduction in the transmission of MDROs. Therefore, I shouldn’t think many ICUs will be rushing to implement universal gloves and gowns on the strength of these findings.
