The prevalence of CP-CRE can be eye-wateringly high in some parts of the world. In Greece, for example, the rate of carbapenem-resistance in invasive K. pneumoniae isolates was 70% in the latest EARS-Net data. In the USA, one study from a long-term acute care facility in California found that almost 50% of patients were colonised. The picture is very different in the UK, with a very low prevalence of CPE reported in most studies as illustrated by the systematic review and meta-analysis that we’re going to look at today.
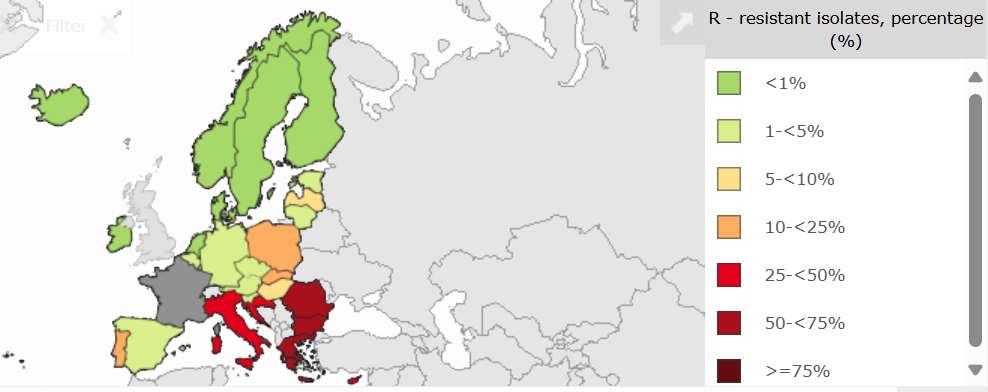
If we look across Europe, we can see considerable variation in the prevalence of carbapenem-resistance in invasive K. pneumoniae isolates, ranging from virtually 0% in the Nordics to >75% in some regions (see the figure below). UK data hasn’t been included in this database since Brexit (thanks Brexit!), but if it were included, the UK would definitely be in the green, with <1%.
Surveillance: What we know and what we don’t
I was a collaborator on this systematic review with colleagues from Imperial. We set out to determine the prevalence of CP-CRE. The review analysed 32 studies involving over 1.1 million participants and nearly 700,000 bacterial isolates. Most of the data came from England, and the majority of studies focused on hospital settings. Only two studies examined CP-CRE in the community, where prevalence was estimated at just 0.1%. Whilst this is encouraging, the lack of solid community data is a major gap—especially considering the potential for discharged patients to reintroduce CP-CRE into non-clinical environments.
Interestingly, the prevalence of CP-CRE identified through universal hospital screening (0.9%) was comparable to that found through targeted screening of high-risk patients (1.2%). This raises questions about the effectiveness of current risk-based screening strategies. Are we using the wrong risk factors, or just applying them badly?
The COVID-19 effect
The pandemic disrupted routine CP-CRE screening in many hospitals. While reported cases dropped, this may reflect reduced hospital admissions and a temporarily different population of patients (generally younger and without the traditional risk factors) along with interrupted surveillance rather than a true decline in prevalence. Some hospitals paused CP-CRE screening altogether, and it’s unclear whether those programmes have been fully reinstated. This interruption could have long-term consequences for IPC compliance and effectiveness (thanks COVID-19).
Implications for IPC policy and practice
Is it time for a national audit of CP-CRE screening strategies? This would help identify gaps in compliance, assess the impact of the pandemic, and inform updated guidelines. For example, introducing pre-discharge screening could help prevent carriers from re-entering the community undetected. I also think it’s time for focussed point prevalence surveys in higher risk patient populations, where prevalence and risk may well be higher.
The review also highlights the importance of consistent laboratory methods and screening protocols. Variability across studies makes it difficult to compare results and track trends. Standardisation is essential if we’re to build a reliable national picture of CP-CRE prevalence.
Where is CP-CRE in the UK?
This question slightly depends on where you are in the UK! If you’re in the Northwest (especially the Greater Manchester region) you probably won’t be asking this question! But other parts of the UK will see hardly any cases, especially of clinical infection. Part of this difference is driven by variation in sampling and laboratory practice, and there’s work to do here. But my best guess is that control on antimicrobial prescribing in hospital and non-hospital settings is the root cause for the relative low prevalence of CP-CRE in the UK, the variation of CP-CRE prevalence across Europe, and the pockets of very high prevalence in some parts of the world.
Looking ahead
This is the first systematic review to synthesise CP-CRE prevalence data across UK healthcare and community settings. It provides a valuable foundation for future research and policy development. But it also makes clear that we need more data—especially from community settings—and more consistent screening and laboratory practices.
Discover more from Reflections on Infection Prevention and Control
Subscribe to get the latest posts sent to your email.