As we bid farewell to 2024, a time for reflection, objective setting, and the odd new years resolution to break early in 2025. The latest ESPAUR report was published a few months ago, and helps us to set some priorities for 2025 and beyond. As ever, there’s a mixture of good news and bad news in the report, but mostly I’m grateful that we have sufficient data and co-ordination to give us this level of detail about the current and emerging threats related to HCAI and AMR in the UK.
Here are some highlights and points for discussion:
- Levels of AMR have surpassed the pre-pandemic peak of 2019 for the first time, with the Enterobacterales (including K. pneumoniae, E. coli etc) accounting for 83% of the AMR bacteria. In short, we need to keep focussed on the threat from AMR Gram-negative bacteria (whilst not losing sight of the Gram-positives).
- AMR continues to vary by ethnicity, as illustrated by the 2x rate of AMR bacteria in BSI in Asian vs. white ethnic groups. AMR also continues to vary by deprivation, disproportionately affecting the most deprived areas.
- Although only half the story clinically*, the crude 30-day mortality from a CPO infection in a sterile site was 23%, and the rate of CPO from sterile sites have doubled since 2021.
- Rates of Candidozyma auris (C. auris) remain low in the UK (although I suspect we will see more develops on this in the 2025 version of the ESPAUR report!). London and the South East seem to be emerging as hotspots, with 50 cases reported in 2023.
- Antimicrobial prescribing continues to increase in primary care and decrease (very slightly) in secondary care.
- There’s a cool set of infographics published alongside the report, here. As an example, here’s the infographic from the HCAI PPS.
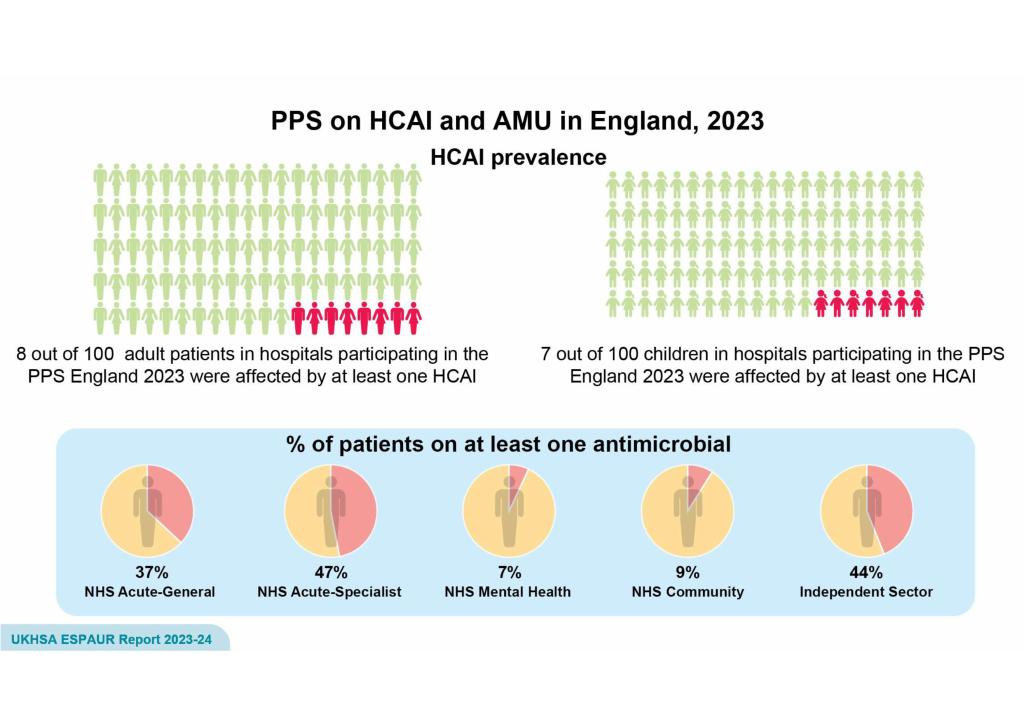
The HCAI PPS found that 7.6% of inpatients had an HCAI. This is slightly higher than the 6.6% found in 2016 – but difficult to know whether one percentage point difference is significant. Prevalence of HCAI in acute hospitals was 8.0% (see Figure 4.2, which clearly illustrates these differences). 37% of inpatients in acute hospitals were on an antimicrobial, and 47% in specialist centres. This was similar to the 2016 PPS. In terms of devices, 7% of patients had a central line, 42% had a peripheral line, and 19% had a urinary catheter. All of this powerfully illustrates the challenges we face as we move into 2025.
Finally, a quick thank-you for reading during 2024, and look forward to seeing you next year.
* By this I mean that patients who develop an AMR infection usually have many co-morbidities that may them more likely to die from other causes.
Discover more from Reflections on Infection Prevention and Control
Subscribe to get the latest posts sent to your email.