I was delighted to spend a day at the FIS International 2025 conference in Bournemouth this week to collect my HIS Early Career Award. I had a the honour of an award lecture – you can download my slides here.

If you’ve ever had to write an award lecture, you’ll know how difficult it is to get the right balance between an appropriate degree of focus on your own work, a consistent narrative, and something that will actually be interesting to listen to! I had a couple of false starts, but ended up focussing on three areas of research where I’ve had the privilege to contribute to (environmental contamination, MRSA, and VRE), a little bit about my career, some lessons I’ve learned along the way, and finally outlining some of my own research priorities (see image below).

The role of the environment in the transmission of HCAI
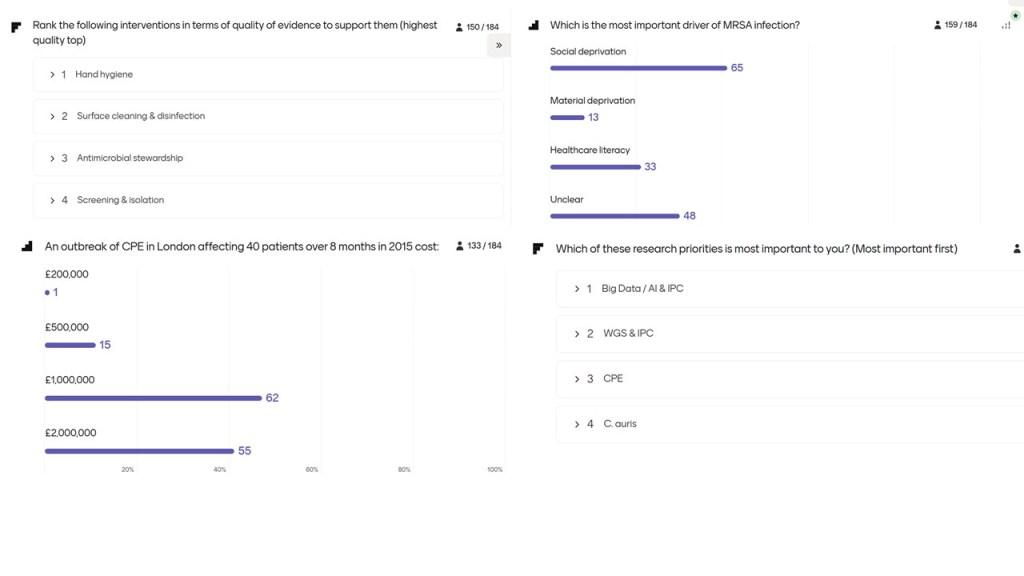
I started off asking the audience about the strength of the evidence base to support the following key IPC interventions: hand hygiene, surface cleaning/disinfection, antimicrobial stewardship, and screening/isolation. To my slight surprise, hand hygiene came out top in the ranking, whereas I now think there’s higher quality evidence for interventions to tackle inanimate surface contamination (that’s not to say we shouldn’t do hand hygiene and the rest too)!
To this day, more than 25 years later, a study where cauliflower DNA was inoculated onto the telephone receiver in a neonatal ICU pod remains one of the most compelling demonstrations of the potential role of surface contamination in the spread of pathogens that can cause HCAI. It demonstrates the rapid spread, extend of spread across the unit, and dynamic interchange between hand and surface contamination. Its no surprise then that the MDRO status of a prior room occupant significantly increases acquisition risk for subsequent patients, with meta-analyses showing odds ratios (ORs) ranging from 1.6 to 4.5 for various pathogens.
This is all underpinned by the extraordinary capacity for organisms (and not just bacterial endospores) to survive on surfaces for extended periods. I touched on two environmental interventions that have been shown to be effective: hydrogen peroxide vapour (which, along with other approaches, has been shown to mitigate the increased risk from the prior room occupant), and increased cleaning of shared medical equipment.
CPE & MRSA
I described my experience of managing an outbreak of CPE at Imperial. The outbreak affected 40 patients over eight months incurred costs approaching £1 million, with major expenditures on screening, contact precautions, and lost revenue from elective procedures.
I also went through a couple of papers that came out of my post doc, focussing on MRSA genomic epidemiology. In one study, whole genome sequencing (WGS) revealed that both community- and hospital-associated MRSA are linked to household deprivation, overcrowding, and recent immigration. In another similar study, inter-hospital transfer further facilitates MRSA transmission across healthcare networks.
My career
I spent a little time describing my career journey. Following 15 years working in the private sector, latterly with a PhD and post-doc part-time, I took the opportunity to join the Imperial IPC team around 10 years ago. During this time, I registered as a Clinical Scientist by equivalence and attained HSST to become a Consultant Clinical Scientist, also by equivalence. This has all allowed me to become the Director of IPC at Guy’s and St Thomas’ NHS Foundation Trust, alongside some research at Imperial College London. I’m incredibly grateful for the opportunities that I’ve had and the guidance I’ve been given by many mentors.
What I’ve learnt along the way…
I thought it would be remiss not to reflect briefly on what I’ve learnt along the way! I found it hard to distil this down to a few points, but I ended up with a focus on behaviour change. Ultimately, this is what we are trying to achieve. Whether it’s a change in behaviour of our front line clinical teams, organisational leaders, or IPC teams themselves, we’re trying to put our priorities higher up the list of busy people! Related to this, the way that we communicate is paramount. If we talk in terms of issues that are meaningful to the individual we’re trying to reach, we are much more likely to actually change behaviour. I also reinforced the importance of strong partnerships – we can only go so far by ourselves and it’s likely that our ‘success’ or otherwise will be determined more by our surroundings and collaborations than by our own individual merit.
Research priorities
I concluded by outlining my own research priorities in the coming years.
- WGS and IPC. WGS, especially when used proactively, has been shown to bring several important IPC benefits: ruling in / ruling out outbreaks, plus much more! But it hasn’t been implemented widely. I plan to evaluate the reasons for this via the GENOTIPE network.
- AI and Big Data: The availability of big datasets combined with artificial intelligence offers unprecedented opportunities for real-time surveillance, outbreak detection, and predictive modelling.
- Emerging pathogens: Candida auris and CPE remain at the forefront due to their resistance profiles and outbreak potential.
Frankly to say that I’m in my early career is a bit of a stretch, let’s be honest. (My family in particular find it hilarious that I’ve got an “early” career award!) But I am genuinely grateful and honoured to receive this award, as a recognition of the small contribution that I have made to our understanding of the prevention and control of hospital pathogens, in conjunction with various different groups and teams.
Discover more from Reflections on Infection Prevention and Control
Subscribe to get the latest posts sent to your email.