 Whilst the organisation of an infection control service isn’t everybody’s cup of tea, it is mine now. So, what are the key elements of a successful programme? A thoughtful review in Lancet ID penned by an all-star cast (including Zingg, Holmes & Pittet to name but a few) provides a framework for answering this question. Their systematic review yielded 10 key components:
Whilst the organisation of an infection control service isn’t everybody’s cup of tea, it is mine now. So, what are the key elements of a successful programme? A thoughtful review in Lancet ID penned by an all-star cast (including Zingg, Holmes & Pittet to name but a few) provides a framework for answering this question. Their systematic review yielded 10 key components:
- Organisation of infection control at the hospital level;
- Bed occupancy, staffing, workload, and employment of pool or agency nurses;
- Availability of and ease of access to materials and equipment and optimum ergonomics;
- Appropriate use of guidelines;
- Education and training;
- Auditing;
- Surveillance and feedback;
- Multimodal and multidisciplinary prevention programmes that include behavioural change;
- Engagement of champions;
- Positive organisational culture.
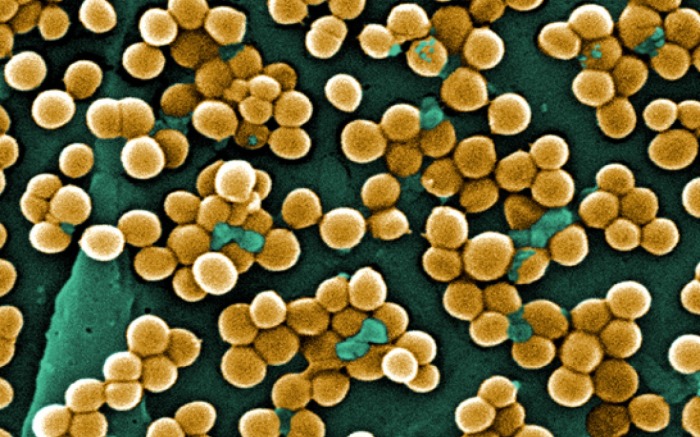
None of these are especially surprising, or that difficult to implement. It’s strange in a way that we know from multiple studies that high bed occupancy results in more transmission (specifically of MRSA). So why don’t we just reduce the rate of bed occupancy? If you account for the extended length of stay for patients who become infected, it would probably result in a net increase in patient throughput. Similarly, understaffing results in more transmission (again, specifically of MRSA). So why don’t we just make sure we hit adequate levels of staffing? I suspect the answer here is short-sighted accountancy combined with a genuine lack of the right staff to fill the necessary vacancies.
I’ve always found it a bit odd that the mere act of performing surveillance and reporting the results back to wards reduces HCAI – but there’s a fair amount of data behind this. I suspect it has to do with the type of people we are dealing with: busy healthcare professionals. If their unit’s rate of MRSA (or whatever) is, in the politest possible sense, in their face, they’re more likely to do something about it.
Finally, nurturing a positive organisational culture is crucial but somewhat philosophical. How do you measure whether your organisation has a positive culture? Perhaps perception is reality here, so the best approach is probably to consider organisational positivity as a highly transmissible infectious agent!
I think you might be interested in obk col 18. What does it take to prevent an outbreak? Not going to be the final title but you get the jist.
LikeLike
People often assume what they are experiencing is the acceptable and the norm until you can show them that it is not
LikeLike
bonjour je suit une infirmière au service de semep épidémiologie et médecine préventive et j aimerais bien de faire une formation sur l’hygiène hospitalière et les infection nosocomiale au niveau de votre hôpital merci
LikeLike
Dear Jon, your blog is very interesting, thanks for sharing your knowledge with the cybercommunity.
I was wondering if you have ever looked into the effects of chlorine dioxide as a bacteria killer and the claims that it can kill various microorganisms including plasmodium (or so says the youtube video filmed in Africa).
Many thanks,
Alessandra
LikeLike