A fabulous study recently published in JAMA evaluates the ‘Benefits of Universal Glove and Gown’ (BUGG) in US ICUs. This is a model study design: one of the first cluster randomized controlled trials of a non-therapeutic infection control intervention. Twenty ICUs were paired and randomized to either universal glove and gowning, or to continue the current practice of placing patients known to be infected or colonized with MRSA and VRE on contact precautions. The hypothesis is that undetected colonization with MRSA and VRE is common, and the only real way to address this is to assume everybody is colonized!
Summary of findings:
- Universal glove and gowning was not associated with a reduction in a composite measure of MRSA / VRE acquisition (the primary outcome).
- VRE acquisition was not reduced by universal glove and gown use, whereas MRSA was.
- CLABSI, CAUTI and VAP; ICU mortality; and adverse events did differ significantly between the two groups.
- Hand hygiene compliance on room entry was not significantly different between the two arms, whereas hand hygiene compliance on room exit was significantly higher in the intervention arm.
- Healthcare workers visited patients 20% less frequently in the intervention arm (4.2 vs. 5.2 visits per hour).
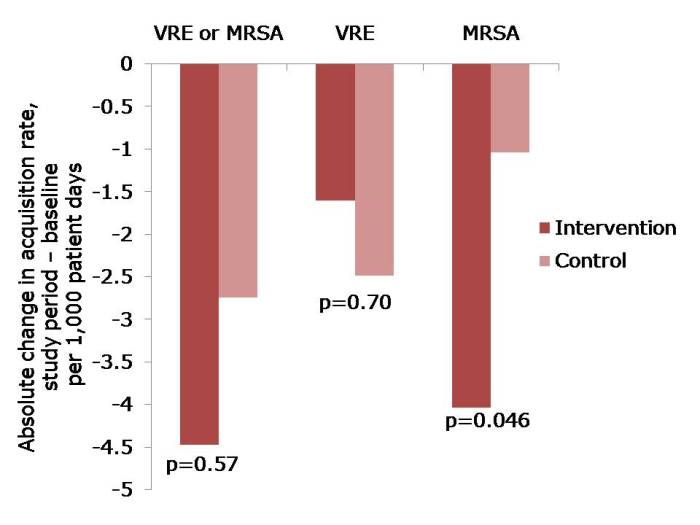 Figure: The change in acquisition rate, comparing the baseline period with the study period for the intervention and control units.
Figure: The change in acquisition rate, comparing the baseline period with the study period for the intervention and control units.
Here’s what’s BUGGing me about this study:
- The acquisition rate in both intervention and control study arms reduced (Figure). The acquisition rate reduction in the control arms may be due to improved compliance with admission screening, resulting in more accurate ascertainment of who required contact precautions.
- The significant reduction was achieved for MRSA but not for VRE. The authors suggest that VRE colonization may have been suppressed on admission and not detected, and flourished during antimicrobial therapy giving the impressive of acquisition. I wonder whether differences in the routes of transmission may also have contributed; for example, VRE seems to be substantially “more environmental” than MRSA. Another potential confounder is that, by chance, the prevalence of MRSA or VRE on admission to the intervention ICUs was more than double that in the control ICUs (22% vs. 9%). In actual fact, the raw rate of MRSA acquisition in the intervention ICUs was marginally higher than in the control ICUs during the intervention period (6.00 vs. 5.94 per 1000 patient days), even though the change in rate was significantly greater on the intervention ICU. Although adjustment was made for this difference in the analysis, it may have skewed the findings somewhat.
- The authors achieved remarkably high compliance with admission screening (around 95%), discharge screening (around 85%) and glove and gowning (around 85%). Each site had the luxury of a study coordinator and a physician champion to lead implementation, plus weekly feedback on screening compliance and visits from study investigators. Most ICUs would not be afforded these luxuries so I suspect that real-world compliance outside of the somewhat artificial study environment would be considerably lower. Indeed, an ID Week poster suggests that compliance with gowning in one US ICU was a ‘dismal’ 20%!
- Adverse events were not significantly higher in the universal glove and gowning arm, which may seem surprising prima facie. However, the reason why adverse events are more common for patients on contact precautions is that they are marginalized by being on contact precautions. If all patients are effectively on contact precautions, the time of healthcare workers would be spread evenly.
- Universal gloving is likely to result in universally bad hand hygiene compliance within the room during patient care; when healthcare workers feel protected, they are less likely to comply with hand hygiene and gloves are a good way to make healthcare workers feel protected. The increase in hand hygiene compliance on room exit is probably also a symptom of inherent human factors, since healthcare workers feel more ‘dirty’ when exiting the room of a patient with a higher perceived risk of MDRO ‘contamination’ (the so-called “urgh” factor).
- Healthcare workers had less time for patient care in the intervention arm because they were busy donning and doffing gloves and gowns. Interestingly, the authors suggest that fewer visits may be a good thing for patients, and may have contributed to their reduced chances of acquiring MRSA. This seems unlikely though, given the fact that VRE acquisition was not reduced. On balance, less contact with healthcare workers is likely to be bad for patients.
- The increased cost of universal glove and gowning was not evaluated and, whilst incrementally small, would be a substantial sum.
In summary, this study sets the standard in terms of rigorous assessment of an infection prevention and control intervention. Universal application of gloves and gowns is unlikely to do as much harm as universal administration of mupirocin, but it will not make a profound reduction in the transmission of MDROs. Therefore, I shouldn’t think many ICUs will be rushing to implement universal gloves and gowns on the strength of these findings.

Universal solutions tend to give universal problems. One of the main problems is that there was lower compliance in hand disinfection because there was a false sense of security. This might cause new and maybe even more trouble.
LikeLike
In actual fact, hand hygiene compliance was no different on room entry and actually higher on room exit in the intervention arm (universal glove and gown). I suspect the higher rate of compliance on room exit is due to perceived risk of hand contamination when gloves are worn (the “urgh” factor). This study did not assess hand hygiene compliance during the patient contact inside the room. If they had, I suspect that overall hand hygiene compliance would have been lower for patient contacts when gloves were worn.
LikeLike
Jon, excellent write up. I agree with your comments. My concern remains a lack of focus or discussion on the impact of the patient experience. Hospitals with universal gown and glove may be perceived as “dirtier” by patients and families. You touch on the impact on care as well. Simple things such as a handshake or touch on the arm can help make connections between healthcare workers and their patients. What happens to this when we start to treat all patients in contact precautions?
LikeLike
Could you argue that having all patients on contact precautions is better than having some patients on contact precautions? Less marginalization of patients on contact precautions?
LikeLike
“I believe if one explained the process and reasoning behind the precautionary measure, most patients and their families would not only jump on board but may become the best advocate for the hospital. In may experience, patients that understand the reasoning behind a decision are much more likely to adopt the idea.”
See: http://www.biomedcentral.com/content/pdf/1472-6963-12-88.pdf
LikeLike
As an industrial hygienist at heart, one element that has always bothered me about universal gloving is the lack of focus on appropriate timing for donning and doffing gloves. Universal gloving tends to lead to universally contaminated gloves. Hand hygiene must be paired with appropriate timing of glove use or it is rather useless.
LikeLike
I agree – gloves can very easily lead to a false sense of security. For this reason, glove use is less common in the UK than in the US. See here for more details: http://www.nhsprofessionals.nhs.uk/download/comms/CG1_NHSP_Standard_Infection_Control_Precautions_v3.pdf
Also, this useful Royal College of Nursing (RCN) guidance provides some detailed information on the timing for donning and doffing gloves: http://www.rcn.org.uk/__data/assets/pdf_file/0003/450507/RCNguidance_glovesdermatitis_WEB2.pdf
LikeLike
I think gloves & gowns should be used to protect HCW
LikeLike
But HCWs are not really at risk of acquiring MRSA and VRE! I think the idea that gloves and gowns are for “self-protection”, although a strong driver for compliance in one sense, is not particularly helpful.
LikeLike
A wonderful summary of a unique study that challenges our understanding of infection prevention and control practice that is mostly based on the introduction of multiple interventions in outbreak situations. What is more interesting is that it was published in JAMA, which is not a forum that infection interventionist and healthcare epidemiologist visit on regular basis. The study confirms what we knew about visits to patients with MDRO and compliance with hand hygiene.
LikeLike
Take the point that not many infection preservationists would read JAMA regularly, but it’s a good thing that such a high-impact journal was prepared to publish a study about a non-pharmaceutical infection control intervention. This is quite a coup for the authors and, by proxy, the profession!
LikeLike
With the realization that people will do what is easiest, not necessarily right, healthcare must take steps to identify patients who, as you so succinctly detailed above, are infected, colonized, or have a high index of suspicion for the need to implement contact precautions. In the long run, a $300 nares or perianal swab test will be most beneficial and cost effective. Even with group purchasing organizations, the cost of disposable gowns is in the $0.65 to $0.88 each range. When viewed as a whole – gowns, gloves, disposal costs, time invested, ordering costs, etc., it is most likely more cost effective to use targeted PPE use than universal downing. Proper hand hygiene and proper environmental processing for the ICU and all areas of a healthcare facility may arguably be the best investment.
I should also add that your comment “they (patients) are marginalized by being on contact precautions” is so spot on that healthcare must take steps to not marginalize patients, not remove their independence, not remove their dignity, and not set them up as a disease or infection instead of the person they were before they became a patient and the person they will be at discharge.
LikeLike
Thanks John, the inclusion of some cost estimates for the gowns allows us to put a rough $ value to universal vs targeted glove and gown use. Each ICUs randomized to the universal gloves and gowns had 19 rooms on average, and 4.2 visits per hour. That works out to $1,200 – $1,700 per unit per day (or $450,000 – $610,000 per annum) on gowns alone on the intervention units. This was approximately 10-fold lower on the control units, where only 10% of patients were on contact precautions. If gloves cost a similar amount, you’d be looking at $1,000,000+ per unit per annum in PPE cost alone!
LikeLike
Jon,
Is it possible that your 4.2 visits per hour may be on the low side when one considers that Chaplains, Social workers/discharge planners, housekeeping, dietary (food trays x3), various therapists, and patient care assistants and technicians/nurses aides go into and out of the patient room? On the cost of gloves, that can swing widely, from $0.039 cents each on up. And that is the cost each and two per visit should be used and let’s not forget the large number of gloves that fall on the floors and are disposed of without being used. And some Infection Preventionists insist on disposing of any open boxes of gloves it they are in an isolation room. The costs are enormous.
Just some thoughts.
LikeLike
Ok, so I overestimated the cost of gloves. Using $0.08 per visit for gloves, the total cost for healthcare worker visits alone comes out at $500-$700k per unit per annum for universal gloves and gowns v $50-$70k per unit per annum for targeted contact precautions.It’s not clear from the study whether the audit of ‘healthcare worker’ visits included all personnel or just trained healthcare workers, but I’m pretty sure the cost of gloves and gowns alone would top $1m per unit per annum if you included the other visits that you outline (housekeepers, food deliveries etc).
Interesting that you mention the cost of disposal of unused supplies stored in the room of contact precautions. I was recently involved in an audit of this at Johns Hopkins. We found that the cost of restocking unused, discarded supplies was around $400k per annum on six ICUs: http://www.ncbi.nlm.nih.gov/pubmed/23571363
LikeLike
David Woodard
Director of Infection Control at Valley Health System
I think the BUGG study has great merit, and deserves further controlled clinical evaluation. The basic premise is not unlike “dedicated” equipment currently recommended for management of patients with CDI. In as much as the modes of intra-unit transmission of some “marker” pathogens such as Acinetobacter, or CRE are not totally elucidated, the addition of single use everything deserves consideration.
LikeLike
I agree David in that we should try to explore universal policies. The one caveat is we need to be fairly sure that they won’t do more harm than good in the long run. The universal use of gloves and gowns may prove to be expensive and ineffective in the long run, but it is not likely to do much harm. The same cannot be said for the universal use of antibiotics! http://www.micro-blog.info/2013/06/universal-mrsa-decolonization-will-tend-towards-universal-resistance/
LikeLike